What is Colonoscopy?
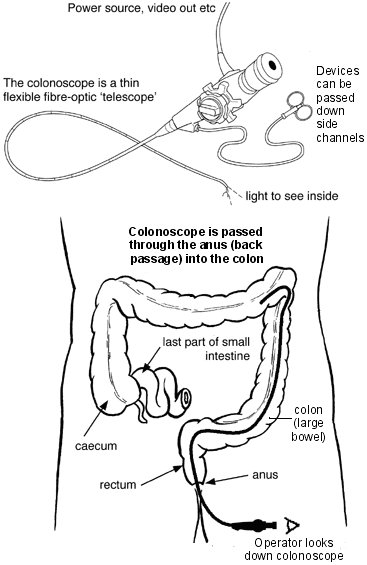
Colonoscopy is a procedure that allows the physician to look directly at the lining of your large bowel (colon) and remove growths (polyps). It is a soft, flexible tube that is one metre long and the size of your finger. A camera on the end of the tube displays an image on a monitor. Colonoscopy usually requires only light sedation and the procedure usually causes little or no pain. Reasons for doing Colonoscopy include screening for colon cancer in patients without symptoms, investigation of bowel symptoms (pain, bleeding, change in bowels, weight loss, positive fecal occult blood test), anemia, follow-up of patients with Inflammatory bowel disease, previous polyps or bowel cancer.
How is Colonoscopy done?
Colonoscopy involves inserting a flexible tube (scope) into the rectum and examining the lining of the colon. On the end of the scope is a tiny camera that projects images on monitors, enabling physicians to see the inside of the colon. As physicians steer the flexible tube through the colon, they are able to spot polyps and remove them with devices passed through the scope. A colonoscopy is usually a simple test that lasts approximately 15-20 minutes. Please arrive 30 minutes before the test and expect to leave about 30-60 minutes after the test. An intravenous sedative will be given by an Anesthesiologist during the test to make you feel more relaxed and comfortable.
Advantages of Colonoscopy
Compared to barium enema, colonoscopy can detect smaller growths. Colonoscopy is the most effective method of detecting and removing polyps. Polyp removal reduces cancer formation (up to 80% in some studies) and permits earlier detection of cancers which gives the patient a better chance for cure.
What are the risks of Colonoscopy?
A screening colonoscopy is very safe. The Endoscopist who will be performing the tests is experienced and has special training in doing these procedures. However, as with any test, there are rare risks involved:
- Pain: This can occur during and after the procedure. This is caused by stretching of the bowel and inflation of air during the procedure. This usually lasts only a brief time.
- Perforation (puncture of the bowel): There is a risk of approximately 1 in 5000 for colonoscopy screening but increases to 1 in 1000 if polyps are removed. If this occurs, an operation will be necessary involving a stay in hospital for several days.
- Hemorrhage (bleeding): Bleeding occasionally occurs (1 in 5000) if polyps are removed or if biopsies are taken. If the bleeding cannot be controlled, a blood transfusion may be necessary, and occasionally, surgery may be needed.
- Cardiac arrest and death: This is extremely rare (less than 1 in 100,000.) Staff at the clinic are trained to manage this very rare problem.
- Drug reaction: Occasionally patients may have adverse reactions to the drugs administered during the procedure. To reduce this risk, you must let the doctor and nurse know of any allergies you may have to medications.
What are the Alternatives?
It is important that you are aware of the different screening modalities that are available:
- Fecal occult blood stool testing (FOBT): Less invasive tests, but also less accurate (30-60%) than colonoscopy (94%) for detecting colon cancer. If abnormalities are found on stool testing, a colonoscopy is usually required for further evaluation.
- Barium Enema (x-rays): This test involves inserting a special liquid (barium) into the colon that shows up on x-rays. This may miss up to 25% of lesions less than 1.5cm in size.
- Flexible Sigmoidoscopy: Must be combined with a Barium Enema for adequate screening. Less reliable than colonoscopy.
- Virtual Colonoscopy: This form of screening uses a computed tomography (CT) scan to generate an image of your colon.
Before the Procedure
The colon must be cleaned out completely. It is essential that the instructions for cleaning out the bowels are followed carefully. If your colon is not properly cleaned out, the test may need to be rescheduled. A full description of the preparation will be either given to you by your family doctor or can be viewed and printed from our website. (See Patient Forms & Handouts)
When you arrive at the clinic, please see one of our receptionists at the front desk. Please arrive at the clinic half an hour prior to your scheduled procedure. At this time, you will have an opportunity to complete the Patient Information Form if you did not complete it prior to your visit. You will also be given a Consent for Procedure Form to review. One of our nurses, an Anesthesiologist, and your Endoscopist will meet with you prior to the procedure to verify your identity and the procedure which you are having, the success of your preparation, review your medical history, and answer all of your questions, including about the procedure and consent.
Once all of your questions have been answered and the Consent Form is completed, the Anesthesiologist will start an intravenous line in preparation for the procedure and sedation. The procedure Nurse will attach monitors to allow the team to watch your vital signs during the procedure.
At the Time of the Procedure
The Anesthesiologist will give medications to sedate you and reduce pain and discomfort. The Endoscopist will insert the scope and examine the lining of your colon. The main objective is to safely examine the colon for polyps. If these are found, and are suitable for treatment with the colonoscopy, they are removed at the same time with a snare or biopsy forceps and sent to the lab for analysis. The procedure takes from 15-30 minutes to complete. Your vital signs are monitored regularly during the procedure.
After the Procedure
After the procedure, you will be transported to our recovery area. You will be cared for in the recovery area by our recovery nurses until the effects of the medication have worn off. During this time, your vital signs will be monitored to check your progress. After the effects of the sedation have begun to weaken, your doctor will come to speak to you and inform you of the results of your colonoscopy. You will also be given written instructions about how soon you can eat and drink, plus other guidelines for resuming your normal routine. A follow-up appointment will be made to discuss any lab results, if necessary. A detailed letter of the procedure and outcome will be forwarded to your family doctor within 7 business days.
You Must Be Accompanied Home By A Responsible Adult. You Cannot Drive A Vehicle Or Operate Machinery For The Rest Of The Day. You Are Advised Not To Make Any Important Decisions Or Sign Any Documents For The Rest Of The Day.
